Imalariya
| Imalariya | |
|---|---|
 | |
| Uhlelo nezibonelelo zangaphandle | |
| ICD/CIM-10 | B50-B54 B50-B54 |
| ICD/CIM-9 | 084 084 |
| OMIM | 248310 |
| DiseasesDB | 7728 |
| MedlinePlus | 000621 |
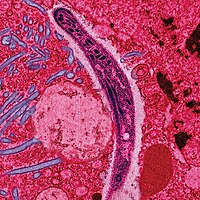
Imalariya sisifo esisuka kwiingcongconi esosulelayo esiba sebantwini nakwezinye izilwanyana esibangelwa zizimfimfithi-gazi (uhlobo lweseli enye izinambuzane) zePlasmodiyam.[1] Imalariya ibangela iimpawu ezidla ngokuquka ifiva, ukudinwa, ukugabha intloko ebuhlungu. Kwiimeko ezimandla inokubangela ulusu olutyheli, ukugula, ikoma okanye ukufa.[2] Ezi mpawu zidla ngokuqala kwiintsuku ezilishumi okanye ezilishumi elinesihlanu emva kokuba ulunyiwe. Kwabo bangakhange banyangwe kakuhle isifo sinokuphinda sibuye kwiinyanga kamva.[1] Kwabo basandul' ukusinda kwisifo, ukosuleleka kwakhona kudla ngokubangela iimpawu ezingekho mandla noko. Oku kukhuseleka kwexeshana kudla ngokuplhela ngokuhamba kweenyanga ukuya kwiminyaka ukuba akuchanabeki ngokuqhubekayo kwimalariya.[2]
Ngokuqhelekileyo, esi sifo sidluliselwa kukulunywa yimazi yengcongconi Anopheles enesi sifo. Oku kulunywa kufaka izimfimfithi-gazi ezikumathe engcongconi kwigazi lomntu lowo.[1] Izimfimfithi-gazi ziya esibindini apho zithi zikhule zize zizale. Iindidi ezintlanu zePlasmodiyam zinokosulela zize zisasazwe ngabantu.[2] Ubukhulu becala ukufa kunokubangelwa yiP. falciparum eneP. vivax, P. ovale,kunye P. malariae ngokuqhelekileyo ibangela uhlobo olungekho mandla lwemalariya.[1][2] Udidi P. knowlesi alufane lubangele isifo ebantwini.[1] Imalariya idla ngokufunyaniswa ngohlolo lwemayikroskopu lwegazi kusetyenziswa iifilimu zegazi, okanye ezine-antigen uvavanyo olukhawulezileyo lokufumanisa.[2] Iindlela ezisebenzisa iziganeko ezilandelelanayo zepolymerase zokufumanisa iDNA yezimfimfithi-gazi ziye zaveliswa, kodwa azisetyenziswa ngokubanzi kwiindawo apho imalariya igqugqisileyo ngenxa yeendleko zayo nokuntsonkotha kwayo.[3]
Ingozi yezifo inokuncitshiswa ngokuthintela ukulunywa yingcongconi ngokusebenzisa inethi yengcongconi kunye nezinto zokugxotha izinambuzane, okanye ngeendlela zokulawula iingcongoni njengokutsutsuza zinto zokubulala izinambuzane nokuvula iidreyini zamanzi amileyo.[2] Kukho amayeza awahlukeneyo okuthintela imalariya kubakhenkethi abaya kwiindawo ezigcwele esi sifo. Ukufumana la mayeza ngamaxesha athile sulfadoxine/pyrimethamine kuyanconyelwa kwiintsana nasemva kwekota yokuqala yokukhulelwa kwiindawo ezinengozi enkulu yemalariya. Nakuba kukho imfuneko, asikho isitofu esisebenzayo, nakuba kuqhubeka kusenziwa imigudu yokusivelisa.[1] Unyango olunconyelwayo lwemalariya ngumxube wamayeza alwa nemalariya aquka i-artemisinin.[1][2] Iyeza lesibini linokuba yimefloquine, ilumefantrine, okanye isulfadoxine/pyrimethamine.[4] Quinine kwakunye nedoxycycline inokusetyenziswa ukuba i-artemisinin ayifumaneki.[4] Kunconyelwa ukuba kwiindawo apho esi sifo sixhaphakileyo, imalariya iqinisekiswe ukuba kunokwenzeka ngaphambi kokuba iqale ukunyangwa ngenxa yenkxalabo yokwanda kokuxhathisa amayeza. Amayeza amaninzi alwa nemalariya sele iwaxhathisa; ngokomzekelo, exhathisa ichloroquine P. falciparum sele inwenwele kwiindawo ezininzi ezinemalariya, yaye ukuxhathiswa kwe-artemisinin sele kuyingxaki kwezinye iindawo zoMzantsi-mpuma Asia.[1]
Esi sifo sinwenwele kwiiTropiki kunye nemimandla esezantsi kwetropiki ekhoyo ngokubanzi engqonge i-ikhweyitha.[2] Oku kuquka ummandla omkhulu [weAfrika Esezantsi KweSahara]], iAsia, kunye [ne[Latin America]]. IWorld Health Organization iqikelela ukuba ngo-2012, kwakukho abantu abazizigidi eziyi-207 ababenemalariya. ngaloo nyaka kuqikelelwa ukuba esi sifo sabulala phakathi kwe-473,000 ne-789,000 yabantu, uninzi lwabo ingabantwana baseAfrika.[1] Imalariya idla ngokunxulunyaniswa nobuhlwempu yaye inefuthe elingelihle kakhulu kuhlumo loqoqosho.[5][6] EAfrika kuqikelelwa ukuba ibangela ilahleko eyi-$12 bhiliyoni USD ngonyaka ngenxa yeendleko zonyango, ukungakwazi ukusebenza negalelo layo kukhenketho.[7]
Iimbekiselo
[tshintsha | Yenza izilungiso kokubhaliweyo]- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 "Malaria Fact sheet N°94" WHO March 2014 retrieved 28 August 2014
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Caraballo, Hector (May 2014) "Emergency Department Management Of Mosquito-Borne Illness: Malaria, Dengue, And West Nile Virus" Emergency Medicine Practice 16 (5)
- ↑ Nadjm B, Behrens RH (2012) "Malaria: An update for physicians" Infectious Disease Clinics of North America 26 (2): 243–59 PMID 22632637 doi:10.1016/j.idc.2012.03.010
- ↑ 4.0 4.1 Organization, World Health (2010) Guidelines for the treatment of malaria (2nd ed. ed.) Geneva: World Health Organization p. ix ISBN 9789241547925
- ↑ Gollin D, Zimmermann C (August 2007) Malaria: Disease Impacts and Long-Run Income Differences (PDF) Institute for the Study of Labor
- ↑ Worrall E, Basu S, Hanson K (2005) "Is malaria a disease of poverty? A review of the literature" Tropical Health and Medicine 10 (10): 1047–59 PMID 16185240 doi:10.1111/j.1365-3156.2005.01476.x

- ↑ Greenwood BM, Bojang K, Whitty CJ, Targett GA (2005) "Malaria" Lancet 365 (9469): 1487–98 PMID 15850634 doi:10.1016/S0140-6736(05)66420-3


